The Journey Towards a New Learning Environment
Imagining what the physicians of tomorrow will be demands dynamic curricular change at the forefront of medical education. While many aspects of medical education remain rooted in tradition, at the Saint Louis University School of Medicine, the past few years have brought about several innovative and compelling curricular changes—including the introduction of new "learning communities," a transition to peer- and team-based learning, and less reliance on the didactic lecture.
Led by Chad Miller, M.D., senior associate dean for undergraduate medical education and professor of internal medicine, recent medical students at SLU have encountered a much different education experience—one that accounts for a wide range of learning preferences and provides students with a deeper sense of what being a doctor means.
From studying the ethics of care and racial bias in medicine to promoting a growth mindset in students, the new curriculum at the School of Medicine paints an inventive and energizing portrait of where medical education is headed.
The Changing Landscape of Medical School

When Dr. Miller began in his current role at SLU in 2017, he faced a significant journey: to modernize the School of Medicine curriculum and ensure it was aligned with the forward direction of medical education.
After a careful evaluation of the curricula, Miller realized that didactic lectures weren't the most effective use of time—for both students and faculty—and this realization led to the creation of new programs in support of active learning.
"We've shifted away from live lectures to 'active learning,' which is rooted in adult learning theory," Miller explains. "These are hands-on activities representing how a doctor might think, behave, or act in a given scenario. Students bring their knowledge and apply them to clinical scenarios where they are actively engaged in thinking through the problem. It is significantly different from the didactic lecture, which can be much more passive."
Neal Weber, former director of instructional design and assessment, prioritized active learning and a learner-centered curriculum due to the sheer amount of content that is presented and expected to be retained. "I had to instructionally rethink how we do things because we had a lecture-centered focus for the curriculum in the past," he says. "Instead of giving them all this content, we need to help them convert their information sustainably."
Curriculum changes instill the importance of collaboration, mutual support, and lifelong learning—an arsenal of skills that serve clinicians throughout their entire careers.
"Medicine is a team sport, regardless of what specialty you go into," Weber says. "We want to get students to be able to work in a team on many different levels."
Engaging with the expertise of colleagues requires respect, humility, and active listening skills—traits Weber believes that many of SLU's active learning programs will nurture. Through this collaborative coaching process, Weber emphasizes the importance of a growth mindset. To foster this, however, students must be presented with the opportunity to fail: "When you're uncomfortable, you learn. When you say, 'I don't know the answer,' that's okay."
By giving students opportunities to have "small failures," Weber explains, they build the capacity to adapt, adjust, and return to their notes to fill any gaps with knowledge. This process, Weber says, is one that clinicians do every day—and it's one that translates to added confidence for students.
A Fresh Start

For new students beginning their first foray into medicine, the entire first year of medical school has been reimagined. Traditionally, medical students would take a series of classes centered on the standard structure and function of the human body—and these classes were typically organized by their various subdivisions: anatomy, histology, embryology, physiology, and so on.
However, the updated course curriculum transforms this approach and organizes each class section by organ. "Anatomy, physiology, histology, and embryology all align in such a way so when we're teaching the anatomy of the heart, we're also teaching the physiology, the embryology, and the histology," Miller says.
Miller hopes that this shift will make the content more resonant for students to retain as they transition to the next phase of their education—and eventually evolve into practicing clinicians.
"What is it that we want when we have a student graduate from SLU?" Miller asks. "We want them to be able to transition seamlessly into an internship. We want them to have the clinical skills to do that and to have a career in medicine—not only today, but for how medicine will evolve tomorrow."
For many students, that means an ability to engage in self-directed learning, to improve and design their own projects, to use the social determinants of health to inform their work, and to approach medicine from a lens of healthcare ethics. To adequately prepare students for long-term success, Miller and the entire SLU faculty have devoted their energy to developing innovative new courses and frameworks: team-based learning, peer instruction, and patient interactions, among others.
Team-Based Learning and Peer Instruction

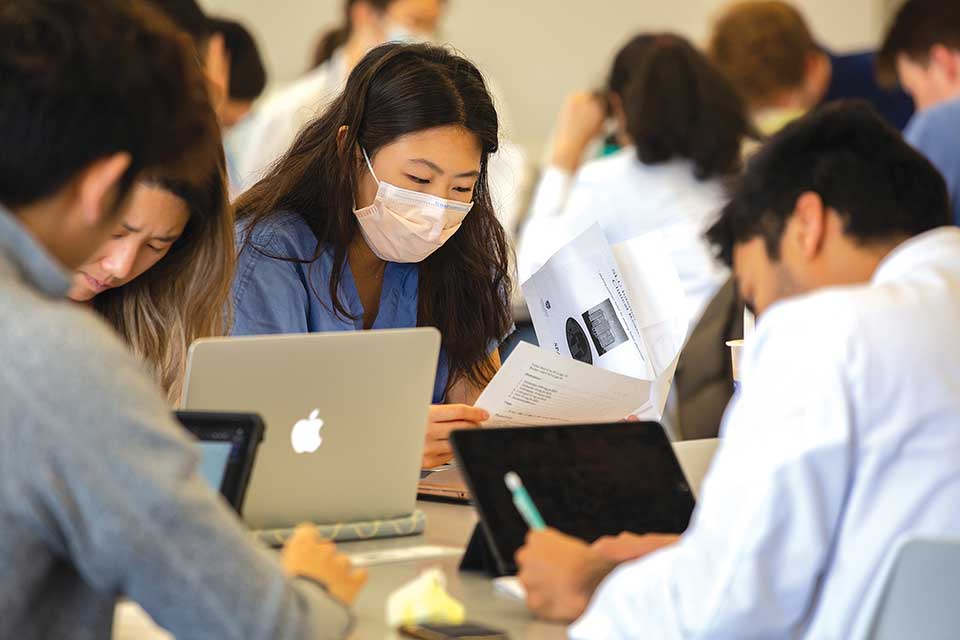
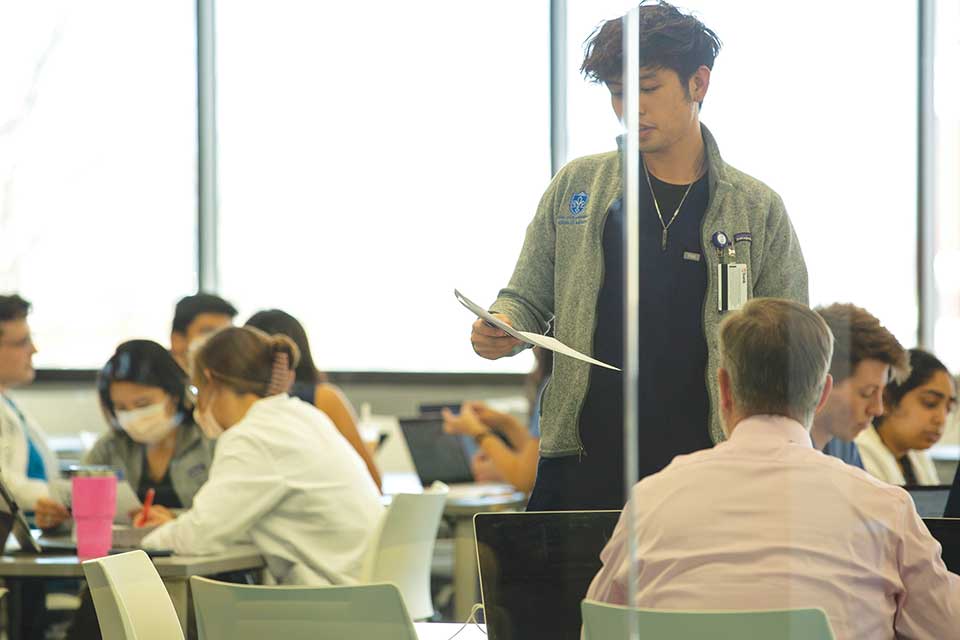
One of the newest initiatives at the School of Medicine—team-based learning—prioritizes hands-on collaboration and mutual discussion between classmates.
In these scenarios, an entire class is brought into one room and split into small groups of six to walk through a clinical case. Led by a faculty member, students work together to learn the nuances of clinical medicine. "It's very different from just passively receiving the information from a lecturer. In team-based learning, they are actively engaged working through clinical problems," says Miller.
A second recent curriculum transformation is peer instruction, whereby students are tested on a series of questions, which helps the instructor get a baseline for student comprehension. If the class threshold is below 70 percent, students consult their classmates for support and explanations. Once they discuss the question with their peers, students are reassessed. "If we cross the threshold at that point, we move on to the next question," says Miller. "If not, then the faculty member slows down and teaches that gap in knowledge to the entire class."
Peer instruction serves as a powerful, effective way to see gaps in student knowledge—while also ensuring that any well-understood concepts are not overtaught.
Preparing for Hands-On Patient Interaction
With the help of artificial intelligence (AI) and virtual reality (VR), the SLU School of Medicine is embracing the future of technology—and preparing students for a lifetime of patient-doctor interactions.
One new initiative is a partnership with PCS Spark, a VR and AI program that allows students to interact with a virtual patient and receive an automated performance assessment. "The student will open up the patient scenario on the computer and see a patient sitting across the room," says Miller. "Through natural language processing and artificial intelligence, they can talk to the computer and take a medical history from the avatar." Since the process is virtual, students can practice this patient-doctor interaction many times. "A student can work on this computer program at any time and get numerous repetitions taking a patient history," says Miller.
Students at SLU also gain hands-on and team-based live training at the Simulation Center (SIM), using rubberized dummies. "You can listen to the heart and lungs and get vital signs from them," says Miller. "We also have task trainers where you can practice putting in an IV line, doing a lumbar puncture, or intubating a patient. We can create a physical simulation scenario to replicate real medicine and allow the students to work through clinical problems in a safe environment where they receive real-time feedback." Dr. Tina Chen, assistant dean of simulation, has been key in building a robust curriculum in simulation at SLU.
The Clinical Skills Center (CSC) brings in paid actors—many of whom are former medical professionals—to help train students. "They'll take on the role of a patient and give the history to the student who does the exam. Then, they'll coach them on what they did right, what they did wrong, and how comfortable they made the patient feel," says Miller.
Upholding Saint Louis University's Mission
Miller believes SLU's recent changes in curriculum go hand-in-hand with elevating the SLU mission, particularly when it comes to the pursuit of truth in the service of humanity.
"The truth in medicine is fundamental," says Miller. "What's the truth from the patient? What is the actual history of what's going on? What is the truth of the disease, and how is it behaving to cause these manifestations?"
For SLU medical graduates, Miller hopes that these questions serve as a frequent touchpoint—and a reminder to pursue the truth relentlessly as they serve humanity. "We want SLU graduates to provide a unique set of skills and a unique outlook on medicine that is different from a non-Jesuit medical school," he says.
"We promote service in everything we do, and we expect it of our students. They will engage in community service while they're here at SLU and approach medicine from a service mindset. We're here to help others—and if those things aren't for the glory of God, I don't know what is."
At the Intersection of Ethics and Communication
For Kimbell Kornu, M.D., Ph.D., assistant professor, and Kyle Karches, M.D., associate professor, medical ethics is not only a profound field of study—but one that is a moral imperative for medical students on the journey to becoming clinicians.
To help students grasp the existential and often unwieldy concepts presented in medical ethics, Dr. Kornu and Dr. Karches developed a new three-year program loosely based on the model of classical education. While today's modern education system focuses on information transfer and technical competence, the classical tradition includes three distinct stages: the grammar stage, the logic stage, and the rhetoric stage.
The Landscape of Medical Ethics
For first-year medical students, the introduction to medical ethics begins with a course devoted to the norms that govern the practice of medicine. Featuring one-hour lectures followed by small group discussions, students become acquainted with new concepts that will eventually become ubiquitous throughout their careers: informed consent, decision-making capacity, withholding or withdrawing treatment, treating minors, and other topics essential to the practice of medicine.
The second year of medical ethics focuses on the logic stage: complex cases centered on different organ systems, which raise new ethical questions and considerations. Based on their foundation in the first year, students become increasingly confident in applying the lens of medical ethics to complicated clinical situations.
Once students reach their third year at SLU, they're asked to practice "micro-ethics," which bridges the divide between technical proficiency and empathetic communication. Students learn how to best communicate with their patients, both verbally and nonverbally. "A big part of being a good physician is knowing how to speak, communicate, and attend to suffering with compassion," says Kornu.
Developing Morally Good Physicians
The goal of medicine, of course, is "to bring about healing," says Karches. "We talk about a good physician as someone who has virtues—which are habits of action that allows them to bring about that healing act in new and challenging circumstances."
This concept extends beyond technical competence: "You have to be able to respond to each patient's unique needs," says Karches. "Some may need certain things from you that others don't, and being able to discern that is part of being a good physician."
"We think of communication today as information going from one source to another source," Kornu adds. "But real communication entails receptivity, and you have to be able to read body language." At its core, medicine is a physician-patient relationship with "two moral agents at work with the singular goal of healing."
Embodying the Jesuit Ethos
The study of medical ethics is deeply intertwined with SLU's Jesuit understanding of service. "The Jesuits don't do a lot of contemplative prayers," says Karches. "They're supposed to be out in the world doing thoughtful things and consistently trying to go into all areas of life and bring thoughtfulness."
While many students early in their careers may feel that their attention should be directed entirely to technical proficiency, studying ethics often leads students to reevaluate this inclination: "You actually have to be just as attentive—and maybe even more so—to the living patient in the room and how you'll communicate with them, how you'll share yourself with them, and how you'll share what you know with them," says Karches.
By broadening the study of medical ethics at SLU, Karches and Kornu hope to narrow the gap between contemplation and action—and make ethics a longitudinal understanding for the duration of a student's career. "Ethics is actually at the heart of what we do as physicians," says Karches. "You can't separate it from learning cardiology or pulmonology or gastroenterology. It's at the heart of it all."
What is it that we want when we have a student graduate from Saint Louis University? We want them to be able to transition seamlessly into an internship. We want them to have the clinical skills to do that and to have a career in medicine — not only today, but for how medicine will evolve tomorrow." — Chad Miller, M.D.
From Students to Clinicians to Advocates
In his landmark course providing an overview of medicine and society, Josh Arthur, M.D., associate professor, offers students a deeper understanding of how the social determinants of health–including income, race, housing, and education–affect a patient's overall health and quality of life.
Helping Students Gain a Deeper Understanding of Place
A pediatrician at SLU, Dr. Arthur recently developed a new course designed for M1 and M2 students, which combines one-hour lectures from subject matter experts followed by a small group discussion session led by a faculty member.
For students new to SLU, Arthur's course provides an in-depth exploration of the history, culture, and access to medical care in St. Louis—and how a patient's health is predetermined by their environment.
The course begins with the history of racism in St. Louis, helping students understand how it creates and perpetuates health disparities. From microaggressions to conscious and unconscious bias, the course unpacks the complicated history of medicine for people of color—and empowers students to gain a deeper understanding and empathy for the challenges and barriers to health that so many patients face.
Arthur hopes that the course will enable students to enter their clinical years, recognizing that if they're not attentive to their patient's social environment, they may find it difficult to improve the patient's health. "That's step one—for them to understand the impact of society and environment on health, and have the tools to build trusting relationships with patients by coming in with compassion, humility, and empathy," says Arthur.
Becoming an Advocate
Advocacy work is intertwined with many of the core themes presented in Arthur's course—and he hopes that his students will leave medical school with the confidence and knowledge to successfully advocate for their patients.
To show students how to speak up as clinicians, Arthur brings a panel of physician advocates to his course. "They speak to the students about how they can take their knowledge, voice, and platform as physicians to act on behalf of patients—at the individual bedside level and at the systemic and institutional level," says Arthur.
"I want them to start having a lens that, when they see an issue with the patient, they can act on behalf of the patient—but they can also think, 'What are the factors that drove this health outcome? And how can I be a voice there?'"
Throughout the course, Arthur includes several different assignments for students. "Some students explore assigned neighborhoods and then come back and report on social determinants of health and health factors they saw in those areas," he says.
Others expanded their awareness by reflecting on the difficulties of accessing proper medical care through the public transportation system; some students opted to write to their local legislators on meaningful topics, such as COVID-19, mask mandates, or reproductive health.
Through these assignments, Arthur hopes students learn to identify a problem, ask the right questions, and remember that their job doesn't end when a patient leaves the room.
"This is a course," he says. "So, it won't teach them everything about the society they live in, but I hope that it will give them a curiosity and a humility that will grow as they become practicing physicians."
