Saint Louis University Researchers Develop New Model by Leveraging an Old Vaccine
Each year, tuberculosis (TB) kills more people than any other infectious disease, and Saint Louis University researchers are working to reduce the disease's impact via vaccine development.
Despite TB’s wide reach and some lost progress during the COVID-19 pandemic, researchers believe it is possible to eradicate TB through advances in vaccine development and public health. To cross the finish line, scientists must find ways to test new vaccines rapidly to prevent TB infections more effectively.
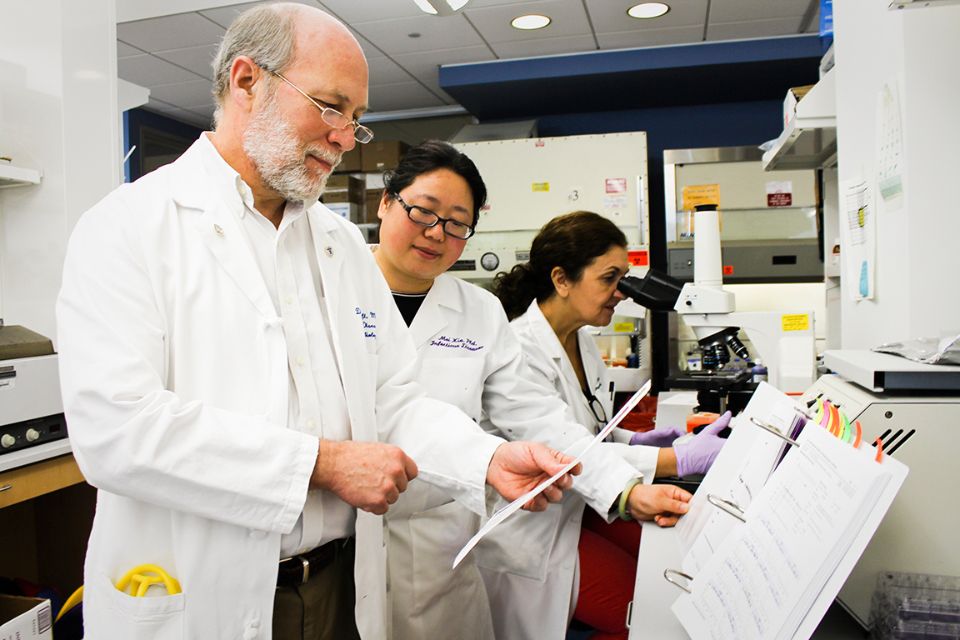
In a paper published in The Journal of Infectious Diseases, Daniel Hoft, M.D., Ph.D., director of the Saint Louis University Center for Vaccine Development, and colleagues from SLU, Emory University School of Medicine, The Emmes Company, LLC, the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health, and New York University Grossman School of Medicine, report a promising new approach to speed up vaccine testing for TB.
Hoft, who also serves as professor and chair of infectious diseases, allergy, and immunology at the Saint Louis University School of Medicine, sought data that could only be gathered by challenging the human immune system directly. This approach, Hoft hypothesized, could provide answers to some TB unknowns. For example, TB animal models do not fully mimic how the bacteria behave in people, and vaccine developers do not have well-defined data about what TB immune responses offer optimal protection against the bacteria.
To test new vaccines, infectious diseases researchers sometimes conduct human challenge studies to quickly learn about how well a vaccine candidate works against an infectious disease, such as influenza. In these studies, researchers first deliver an investigational vaccine or placebo to separate groups of healthy volunteers, and then intentionally infect study participants with a flu virus, all in carefully controlled settings and under close medical supervision, to determine whether the investigational experimental vaccine provides protection compared with the control group. This approach can be instrumental in generating data supporting the approval of novel vaccines.
Mycobacterium tuberculosis, the bacteria that cause TB, however, is too dangerous for human challenge with the fully pathogenic bacteria. The team needed to find another, safer way to challenge the human immune system to find answers to their questions.
Hoft found a workaround in the Bacillus Calmette-Guérin (BCG) vaccine.
The most widely used vaccine in history, with more than 4 billion doses given to patients since 1921, the BCG vaccine contains a live but weakened version of the TB bacteria. The BCG vaccine is given to newborns to reduce their TB risk, but it is less effective against pulmonary TB and often wanes in effectiveness, providing little to no protection in adults.
With the BCG vaccine, Hoft saw a chance to gather data about TB in a human study without the risk of exposing participants to full-strength M. tuberculosis bacteria. To test this idea, the researchers gave 92 healthy adults the BCG vaccine, with participants receiving one of four different doses.
With participants’ immune response to the BCG vaccine serving as a proxy for their exposure to a true infection, the researchers gathered much-needed data about how the immune system responds when it encounters TB.
The team applied a battery of analysis methods to samples collected from the BCG challenge sites and blood, looking for associations between BCG at the injection site, and immune responses as well as gene expression changes in blood.
The findings open up new doors for TB vaccine development.
“Our findings are important for two reasons,” Hoft said. “First, this approach could enable us to screen new TB vaccines early in the pipeline and prioritize the most promising concepts, saving time and money. Second, we have a model to better determine what a new vaccine needs to do to protect against TB. We will be able to identify biomarkers indicating whether new vaccines could better protect someone against TB.”
Among the findings that will help vaccine developers as they create new vaccines:
- Researchers determined that BCG challenge doses of up to 8 x 106 C.F.U. were safe.
- They found that BCG at the challenge sites increases as the BCG dose increases.
- Researchers also identified the most consistent and precise measure of BCG at challenge sites.
- Gene expression analysis found potential biomarkers of immunity that correlated with
inhibition of BCG in people that may provide a TB protective signature.
- They also uncovered immunological and gene expression differences that could underlie the different risks of men and women developing active TB.
- Doctors have long observed that men appear to be more at risk of developing an active form of TB infection, but they do not know why. In this study, researchers found differences in the immune responses of men and women to the BCG challenge, a finding that parallels doctors’ observations with patients who develop the illness.
Researchers hope this new model will help advance our understanding of why men and women have different levels of general immunity.
Hoft is enthused by the findings, which he says could provide a road map for future TB vaccine testing.
“The BCG human challenge model is a promising approach for studying TB immunity,” Hoft said. “The new data will facilitate the vaccine development process, allowing us to make progress toward our ultimate goal of eradicating TB.”
The content in this press release is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.