Taking Steps to Reduce Burnout Among Medical Students
How often do you find yourself feeling depleted of energy? Burnout syndrome is an occupational phenomenon that consists of emotional, physical, and cognitive exhaustion which can manifest due to a multitude of external stressors ranging from illness to adversity. Burnout’s severity can range from mild, where symptoms do not interfere with daily life, to severe, where the affected person is unable to work and feels extreme detachment from their job or education, and can overlap with depression. Burnout syndrome can lead to sleep impairment and emotional dysregulation. This can lead to a vicious cycle of exacerbation, causing depletion of energy. Medical training is filled with long hours of persistent studying and test-taking, potentially subjecting students to intense demands, stress, and exhaustion. Without adequate self-care methods, burnout syndrome can occur.
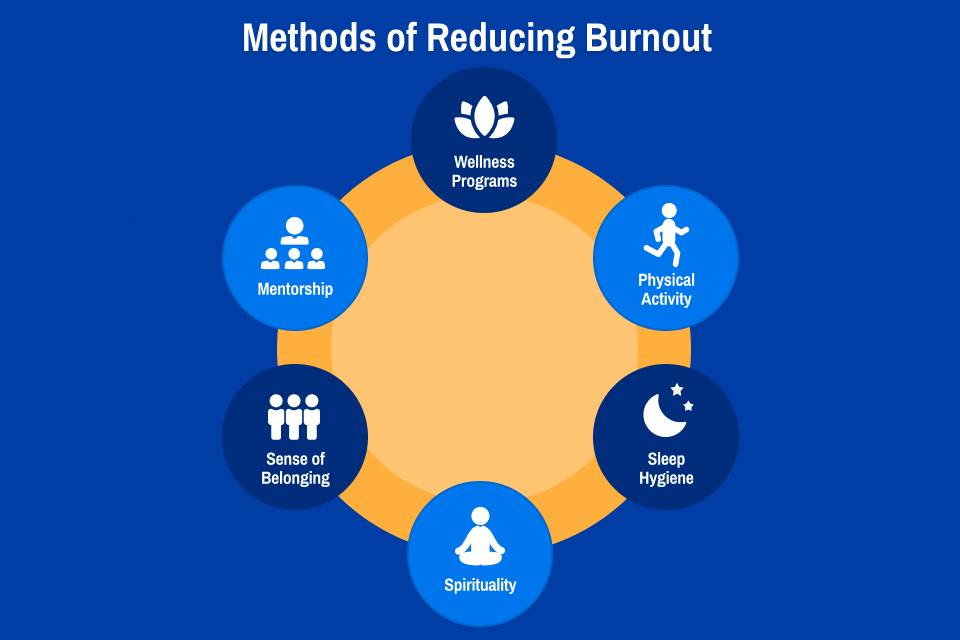
Burnout can begin its development in medical students during the preclinical years, where the pairing of high volumes of information with significant time constraints can lead to limitations in memory. The prevalence of burnout among medical students is estimated to be between 45% and 71%. Unfortunately, burnout can lead to reduced academic performance, decreased professionalism, worsened health, and increased anxiety. Not all medical students seek help or use adequate coping mechanisms, which can lead to adverse long term effects. These include thoughts of suicide, and a decline in empathy, leading to weakened physician-patient relationships. Medical schools can decrease burnout utilizing various institutional strategies including promotion of wellness, physical activity, sleep hygiene, spirituality, and community building.
Curricular changes with the intention to improve students’ mental health are uncommon in medical education. The most common is a transition to pass/fail grading, which can reduce stress and improve student well-being, group cohesion, and satisfaction with education. There is a positive correlation between increased exams and burnout, whereas increasing exposure to patient care tends to decrease burnout. More efficient course content and scheduling, electives, learning communities, and required resilience and mindfulness experiences are associated with lower levels of depression, anxiety, and stress, and increased community cohesion.
Wellness Programs
Initiatives that facilitate student wellness can be effective in reducing burnout. These may include increasing access to mental health care, providing mental health training to faculty, and reducing stigma surrounding mental health. At the University of Hawaii School of Medicine, third-year medical students were offered a program with increased access to counseling services, a “wellness” student handbook, and training on depression for students and faculty. Students in this program had a significant decrease in depression and suicidal ideation, which are often connected to burnout. Implementing similar programs may reduce burnout and improve overall wellbeing among medical students. Wellness programs should work to reduce burdens rather than adding to them, as well as to create an environment that encourages students to recognize burnout and seek help.
Physical Activity
The CDC recommends 150 minutes of moderate-intensity physical activity and two days of strength training per week for adults. Burnout rates were decreased in medical students who participated in aerobic exercise consistent with CDC guidelines compared with those who did not meet CDC guidelines. Students who strength trained according to CDC guidelines also had lower burnout rates than students who did not meet the guidelines. Quality of life was increased in students who met CDC guidelines for aerobic exercise, strength training, or both. Increased physical activity beyond the minimum guidelines was associated with increased benefits. Time and motivational constraints may limit physical activity among medical students. Medical schools may encourage physical activity among students by providing a workout facility on campus, providing allocated time for wellness and exercise, and offering more consistent scheduling.
Sleep Hygiene
Chronic sleep disturbances are a significant contributor to burnout among medical students, as they impair cognitive functioning, reduce emotional resilience, and exacerbate the stress associated with rigorous academic and clinical demands. Medical students can experience more sleep disturbances than other students in the first or second year of medical school. The combination of irregular study schedules, academic pressure, and extracurricular involvement can fuel disrupted sleep patterns. A recent study implemented a practice to set a routine time to wake up and remove electronics at night, finding improvements in sleep quality and reduction in stress. By prioritizing a set sleep schedule and eliminating electronic usage before bed, medical students can attain optimal sleep, leading to increased productivity, improved memory retention, and decreased vulnerability to burnout. Medical schools may contribute by providing instruction to students on sleep hygiene and strategies to obtain quality sleep.
Spirituality
Students with strong spiritual well-being and daily spiritual experiences report higher self-satisfaction and lower rates of psychological distress and burnout. Spirituality is inversely related to exhaustion and cynicism, which both play a role in the development of burnout. Important spiritual experiences among medical students can include connection to God or a higher power, being part of a religious or spiritual community, mindfulness, prayer, or meditation, and other sources of hope or strength. Medical schools can facilitate these experiences through meditation or interfaith prayer rooms on campus, opportunities for spiritual or religious community involvement, and mindfulness activities.
Sense of Belonging
Social support and belonging of medical students are key to overcoming burnout. Students who are isolated can experience increased imposter phenomenon and may perceive their personality and other traits to be incongruous with those of practicing physicians. Specifically, first-year medical students are often expected to act in a specific manner that may be in contrast to their personality. One potential solution is informal peer-assisted learning, which immerses emerges students in social networks and study groups to reduce negative self-evaluation. Through peer engagement, medical students can feel belonging through academic collaboration, motivational support, and overcome mental detachment. Furthermore, finding belonging in an academic setting translates to a professional and a community environment, teaching individuals how to build identity and support in diverse climates.
Mentorship
While a large amount of burnout in medical students can be due to academic stress, medical students can also undergo emotional exhaustion through exposure to human suffering, illness, death, and complex ethical concerns. Without having a mentor to guide processing of these events, students can experience exacerbated feelings of isolation. Furthermore, medical school can create a competitive environment, further discouraging medical students from seeking help from residents or physicians to uphold a strong image. It is crucial that residents and physicians provide empowering mentorship and create a welcoming environment to allow medical students to express their feelings of burnout. Particularly, mentorship provided via positive reinforcement and formative feedback has been noted to improve burnout. Most of all, mentoring programs should encourage strong professional identity formation, helping medical students learn how to ease into the lifestyle of medicine.
Conclusion
Burnout is prevalent among medical students, with long-term effects that stretch beyond academic performance, negatively impacting personal well-being and academic performance. Taking steps to reduce burnout may be difficult due to limited time and motivation among medical students. Densely packed curriculums and financial constraints may prevent medical institutions from properly addressing student burnout. To effectively reduce burnout, medical institutions and students must work together to make necessary changes. Strategies that promote wellness, exercise, sleep, spirituality, and community have shown reductions burnout and improve well-being among medical students.
 Morgan Ford Thorne is a third-year medical student at Saint Louis University School
of Medicine. Ford’s areas of professional interest include pediatrics, program evaluation,
and medical humanities. Ford can be followed on LinkedIn.
Morgan Ford Thorne is a third-year medical student at Saint Louis University School
of Medicine. Ford’s areas of professional interest include pediatrics, program evaluation,
and medical humanities. Ford can be followed on LinkedIn.
 Priyanka Kaushal is a third-year medical student at Saint Louis University School
of Medicine. Kaushal’s areas of professional interest include preventive medicine,
medical education, and advocacy for underserved populations. Kaushal can be followed
on LinkedIn.
Priyanka Kaushal is a third-year medical student at Saint Louis University School
of Medicine. Kaushal’s areas of professional interest include preventive medicine,
medical education, and advocacy for underserved populations. Kaushal can be followed
on LinkedIn.