Vaccine Visionaries
SLU’s renowned scientists are at the forefront of COVID-19 vaccine development.
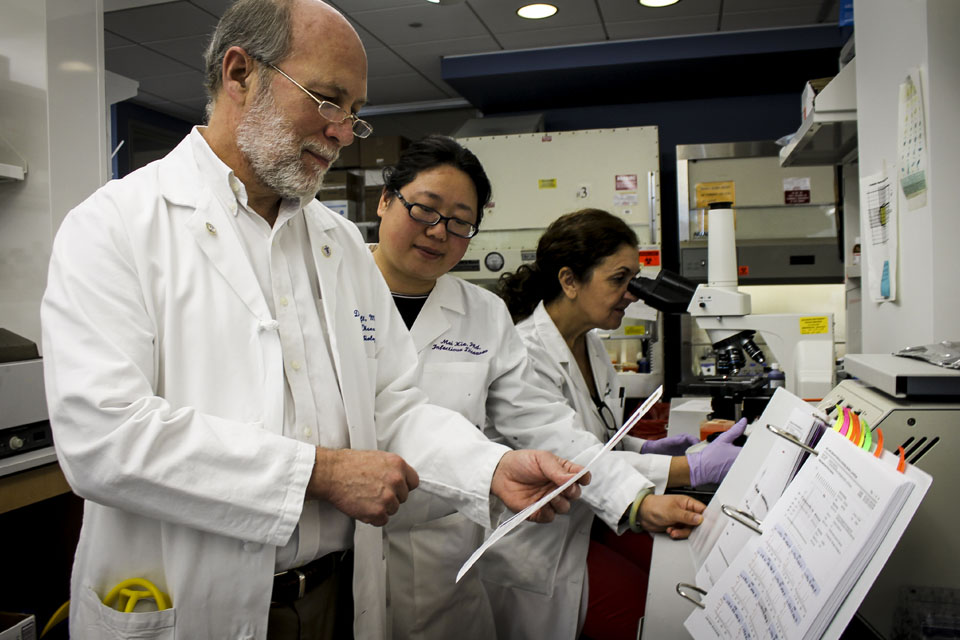
When Dr. Daniel Hoft, professor of internal medicine and director of the Division of Infectious Diseases, Allergy and Immunology, learned in early January that a novel coronavirus was working its way through China, the pathogen hadn’t been identified yet. It wasn’t until a few weeks later that COVID-19 had its name and his team had its mission.
Hoft directs the Saint Louis University Center for Vaccine Development and the Vaccine and Treatment Evaluation Unit (VTEU) — one of only nine centers in the country approved by the National Institutes of Health (NIH) to conduct clinical trials of novel vaccines to protect against pandemic challenges. Hoft, who was appointed in June to the U.S. Department of Health and Human Services National Vaccine Advisory Committee, said many collaborative groups, including the VTEUs, mobilized quickly to decipher the pathogen’s genome and rapidly roll out vaccine trials. In July, SLU’s VTEU became one of the first sites in the country to begin phase 3 trials of the Moderna COVID-19 vaccine.
SLU also was among the 75 sites chosen worldwide by the NIH to evaluate the antiviral drug, remdesivir, in patients hospitalized with COVID-19. This spring, SLU’s primary investigator Dr. Sarah George, associate professor of infectious diseases, allergy and immunology, led clinical trials conducted at SSM Health Saint Louis University Hospital. This trial and those at other sites showed remdesivir shortened the recovery process for patients with advanced COVID-19. In addition, the NIH asked SLU scientists in May to develop a COVID-19 natural history study to explore immune responses in mild, moderate and severe cases of the infection, which will better inform vaccine development efforts.
Both George and Hoft have suspended much of their research on other infectious diseases — including influenza, tuberculosis, Zika, yellow fever and dengue fever — to focus almost exclusively on advancing a vaccine for COVID-19. They have been working overtime, not only on their research, but also to educate the SLU community and the wider public about COVID-19. In this article, they discuss their work and the lessons the world is learning.
Vaccine Development
George: Under normal circumstances, a potential vaccine is initially tested in animal models. The Food and Drug Administration (FDA) usually requires two animal models. If the vaccine proves safe, we move to Phase 1 human trials. We begin testing in healthy adults to make sure there are no safety concerns and the vaccine causes an immune response to develop. Then we go to Phase 2 human studies where we expand the number of healthy adults to look at more people, including sometimes children, adolescents and older adults. If it looks as though the vaccine is safe and immunogenic, we move to Phase 3 human trials, which is field testing. This typically involves vaccinating thousands of people and monitoring them for several years to determine whether the vaccine protects them against the disease being investigated. Under ordinary circumstances, getting a vaccine to market can take 10 to 15 years, but these are not ordinary circumstances. We’re doing everything we can to fast-track development of a vaccine by expediting the timeline for each phase.
Hoft: Under an Emergency Use Authorization from the FDA (which allows the use of unapproved medical products to be used in emergency situations to diagnose, treat or prevent life-threatening diseases), no new animal studies were required before beginning Phase 1 of the COVID-19 vaccine trials.
The animal studies and human studies were conducted in parallel. In one month, scientists compressed years of work. We’re also working with vaccine candidates that we’ve had previous experience with — vaccines that were developed to fight other types of coronaviruses in the past, such as SARS-coV 1. That bypassed a lot of time.
George: The Ebola vaccine was expedited in the same way when we had the horrible outbreak in West Africa in 2014. Scientists did very quick Phase 1 human studies with vaccine candidates they already had. They pulled them off the shelf, so to speak, and then they went straight into Phase 3 studies. The vaccine proved to be protective, and we now have a vaccine against Ebola.
Hoft: In addition, the type of COVID-19 vaccine delivery system we’re using is novel and is allowing us to expedite trials. The system uses RNA [ribonucleic acid, a nucleic acid present in all living cells] as the actual vaccine. Most vaccines are made from antigens — either a protein coming from the pathogen or an entire pathogen that has been weakened in some way and injected into the body to trigger an immune response. The smallpox vaccine and most HIV vaccines are examples of this. Protein-based vaccines can take years to develop because there are more stumbling blocks. Protein-based vaccines require mass production of viral proteins and, in some cases, this can take decades. With the RNA-delivery vaccine, all you need is the sequence of the pathogen’s genome, which the Chinese government shared with the world in January. Instead of viral-based vaccines, an RNA vaccine provides a synthetic RNA encoding a key antigen expressed by the virus, which the body then uses to produce the viral proteins itself. This type of vaccine approach can save months or years.
Contact Tracing
George: Part of the challenge with contact tracing is that this was a new virus unknown to humanity until December. We had to create diagnostic tests from the ground up. That said, there were high-level missteps. We didn’t implement testing soon enough. The World Health Organization had a test available, but the leadership of the United States declined to use it. The Centers for Disease Control had a test that we later learned was defective. It was made in a lab that didn’t meet appropriate standards, so we were weeks and weeks behind. The disease was already here before we could detect it. We have since learned that people were dying in California before we even had the ability to test for the disease. Testing is getting better.
Hoft: We’re learning how important our public health systems are in contact tracing. They need to be functioning optimally and have enough personnel to be able to follow the contact spread as far as it goes. They need to identify infected people, quarantine them and do contact investigation to see where the infection is spreading so we can stop it. These are key to mitigating a pandemic before we have countermeasures, such as vaccines.
Past Pandemics
George: I’ve been an infectious disease specialist for more than 20 years, and this is at least the fourth pandemic I’ve seen in the last decade. We had the flu pandemic in 2009. We get a new flu pandemic every 10 to 15 years so that was expected, and we’re due for another. Then we had the Ebola pandemic in 2014, which caused a global health scare because there were cases spreading to all parts of the world. Fortunately, we never had sustained transmission in the United States for a variety of reasons. In 2015, we had the Zika outbreak — the mosquito-borne virus that caused birth defects in babies. We’ve also had other outbreaks that haven’t hit the shores of the United States but have caused problems globally, such as yellow fever and chikungunya virus. Now we have the COVID-19 outbreak. I have to say this wasn’t a surprise. Certainly, Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, said he was concerned something like this might happen, and it came to pass. This is the largest pandemic I’ve seen because of its sustained transmission.
Hoft: We’ve had three events caused by coronaviruses in the last 20 years or so: SARS-coV 1 in 2002, MERS-coV in 2012 and now SARS-coV 2 — what we’re calling COVID-19. It’s made its way throughout the world, while the other two were completely or mostly contained. COVID-19 appears to be more infectious than the others, and it likely will be seasonal. Many other coronaviruses do circulate seasonally and cause the common cold. COVID-19 is not common, and it’s more dangerous.
COVID-19 Antibodies
Hoft: We don’t have sufficient information to know whether people who have contracted COVID-19 are immune from contracting the virus again. Most researchers, however, believe that infection itself will induce a protective immune response in most people. Otherwise, you wouldn’t clear it. Already we’ve seen in multiple places throughout the world where there have been COVID-19 outbreaks that it seems to slow down at some point. In China, infection has returned to low levels, so now they are focused on people coming into their country with the infection and reintroducing it to the population.
There is circumstantial evidence that suggests infection creates an immune response. How good that immune response is, we don’t know. Most middle-aged people who have a healthy immune response likely will develop a strong immune response to an infection. Immunity should last several months to a year perhaps. We don’t know whether people who don’t have a strong immune response will be as well protected. There’s likely a gradation of immunity.
Role of the Environment
George: We need to have some very real, global-level discussion about how we’re interacting with the environment. A lot of what we’re seeing is a side effect of environmental damage. How did we get the Ebola virus? Where did it come from? It came from the jungles of Africa. We still don’t know exactly what its natural reservoir is, but people are going into the jungles and destroying them. They are killing the native wildlife and eating it. That’s how an outbreak can start. It’s human destruction of an ecological system. The same with the COVID-19. How did we get it? It may have jumped from bats to endangered pangolins that were sold for meat in Chinese markets. If we don’t stop these behaviors, this is going to continue to happen.
Perspective on Pathogens
Hoft: This is the worst acute pandemic in my lifetime. You think about diseases such as HIV, which is a huge problem worldwide, though not as bad in the United States. It has caused about 30 million deaths since it was identified in the 1980s. COVID-19 is the only virus I’ve seen spread throughout the world so quickly and, without countermeasures, has wreaked massive morbidity and mortality. In three months, we went from a virus no one had heard of to an acute pandemic. It’s mind-boggling and definitely is robbing me of sleep. Another huge problem is tuberculosis. It doesn’t spread as rapidly, but it kills more people than any other infectious disease and it’s one of the top 10 causes of death in the world.
George: The NIH has a list of infectious diseases that would keep you up all night, but right now, this is the one keeping me up. We’re all working very long hours. It’s all-hands-on-deck.
Fact vs. Fiction
George: A lot of nonsense exists on the internet. People are hyping treatments that we now know don’t work and may be harmful. I feel a strong responsibility to the general public, my colleagues and my patients to provide good, fact-based information. I advise everyone to stick to fact-based information sources. I also tell people we’re in this for the long haul. Life is hard right now. Life is different. Realistically, we won’t have a vaccine for maybe a year, maybe sooner if we get lucky. Until that happens and the case numbers start to decline, we’re going to have to continue the social distancing as much as possible. Long term, I tell people to try to be optimistic. We should be able to make a vaccine for this, and we will get ahead of this eventually. It’s just not going to be overnight.
Hoft: Every day we’re flooded with more information and new recommendations. It’s a challenge to keep up and to separate fact from fiction. I think it’s wonderful, however, to see how people care about others and are doing everything they can to help, whether it be by following social distancing recommendations or putting themselves on the front lines of caring for patients. Everyone is a hero. It fills me with optimism that the world citizenry is coming together, and we can beat this thing.
Alumni Gift Accelerates Vaccine Efforts
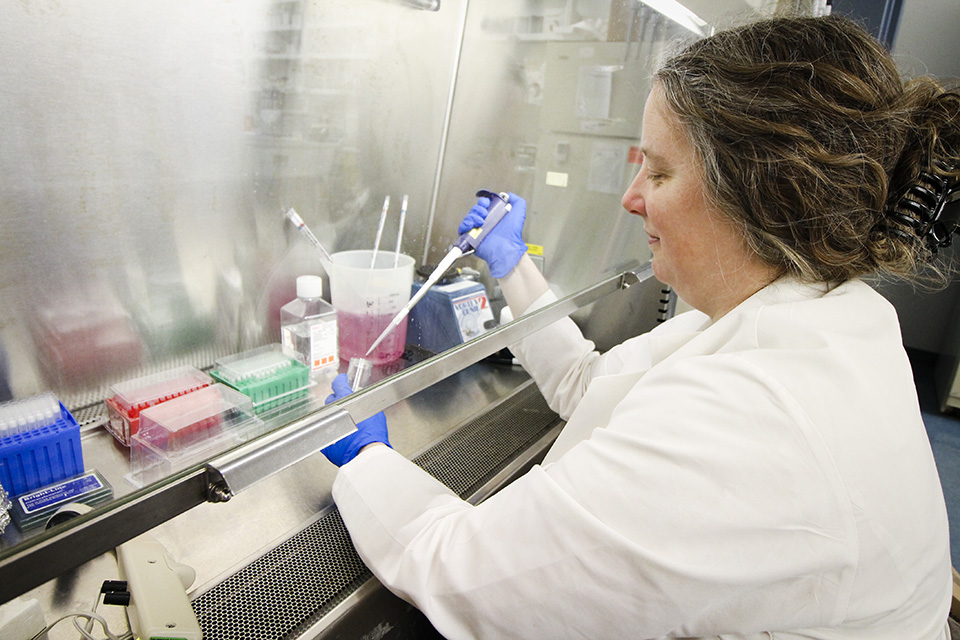
As researchers at Saint Louis University’s Center for Vaccine Development work overtime to find a vaccine to combat COVID-19, they received a generous gift from alumni to fight infectious diseases.
Dr. Stephen C. Peiper (Med ’77) and Dr. Zi-Xuan “Zoe” Wang, his wife, gave $750,000 to SLU to support research aimed at developing new vaccines for COVID-19 and other illnesses. This gift will establish a center of excellence in vaccine research and will be called the Stephen C. Peiper and Zi-Xuan Wang Institute for Vaccine Science and Policy.
SLU President Dr. Fred P. Pestello lauded the couple’s contribution, which supports Saint Louis University’s Accelerating Excellence Campaign.
“I am inspired by Drs. Peiper and Wang’s generosity and investment in the work of leading scientists at Saint Louis University,” Pestello said. “They realize that our infectious disease and vaccine research is second to none. It is gratifying to have successful health care experts in their own right acknowledge the substantial impact science at SLU has on the world.”
Peiper is the Peter A. Herbut Professor and Chair of the Department of Pathology, Anatomy and Cell Biology at Thomas Jefferson University in Philadelphia, and senior vice president for the enterprise pathology and laboratory medicine service line of Jefferson Health System. Wang is the scientific director of the molecular and genomic pathway laboratory for the Jefferson Health System.
Peiper’s scientific work contributed to the discovery of a receptor that allows HIV to be transmitted into cells. A clinical laboratory scientist, Wang is leading COVID-19 testing programs, and her laboratory has provided testing for the 14 hospitals in the Jefferson Health System.
In addition to research on COVID-19, the gift will advance work at SLU to develop new vaccines for other diseases, support a new computational biology team and infrastructure, and assist in recruiting new physician scientists.
For more information or to support SLU’s efforts in vaccine development,
contact Jane Baum at jane.baum@slu.edu.
— By Marie Dilg
Saint Louis University is a Catholic, Jesuit institution that values academic excellence, life-changing research, compassionate health care, and a strong commitment to faith and service. Founded in 1818, the University fosters the intellectual and character development of more than 13,000 students on campuses in St. Louis and Madrid, Spain. Building on a legacy of now more than 200 years, Saint Louis University continues to move forward with an unwavering commitment to a higher purpose, a greater good.