Decades of Research Finally Solve the Quest for RSV Vaccines
The Saint Louis University Center for Vaccine Development led three on-site clinical vaccine trials that helped bring the decades-old mystery of RSV vaccinations to a close.
Every winter, it's the same cold season symphony — a cacophony of coughs, heavy breathing,
and ever-present sneezes. As millions combat the winter season’s recurring illnesses,
many will receive a diagnosis of one of three common respiratory viruses: influenza,
COVID-19, or respiratory syncytial virus (RSV).
Since its discovery in 1956, RSV has been a leading cause of respiratory hospitalizations
in young infants, older adults, and immunocompromised people throughout the world.
Recent years have seen increased diagnoses, hospitalizations, and deaths related to
RSV, with recent studies estimating over 58,000 hospitalizations in children younger
than five years old. This prompted immediate action by researchers to develop a vaccine
that would protect against the virus’s attack on the respiratory system.
An RSV vaccine has been a high priority among vaccine researchers since its discovery. For years, countless studies were conducted with the hopes of discovering a solution to such a contagious infection. When vaccines were ready for trial, Saint Louis University's Center for Vaccine Development was selected to conduct three separate RSV vaccine trials, including two focused on adults and one on children. And in 2023, their work aided in the success of today’s approved Pfizer vaccine by the U.S. Food and Drug Administration (FDA) and subsequent recommendations for use by the Centers for Disease Control and Prevention (CDC).
Yet, the first attempts at vaccine development for RSV were shrouded in a shadow for decades until the recent success cracked its over 50-year-old mystery.
The Darker Days of RSV
As RSV cases surged in the late 1950s, researchers immediately embarked on a plan to develop a vaccine to protect the critical age groups of young children and older adults against the virus. After the success of the polio vaccine in 1955, researchers began experimenting with a process that would create a similar vaccine that would create the necessary antibodies to protect against RSV.
In the mid-1960s, researchers developed a formalin-inactivated RSV vaccine that contained an inactive version of the virus. This was administered to young infants and children in four clinical trials beginning in 1966. But, the initial trials left complete devastation in its wake — resulting in two deaths and the hospitalization of 80% of the infants from enhanced RSV disease (ERD).
Sharon Frey, M.D., professor emeritus in the Division of Infectious Diseases, Allergy and Immunology, served as a principal investigator for two of the three recent vaccine trials hosted at SLU. She explained that the shock of the early trials reverberated through the vaccine development field.
“In the early phase trial, it caused significant adverse events by inducing nonprotective antibody responses that actually enhanced RSV infection and disease,” she said. “This [realization] put a stop to all RSV vaccine testing in humans for several decades.”
The pathologic vaccine response discovered during initial vaccine trials was eventually shown to be caused by a mechanism called antibody-dependent enhancement (ADE) of disease. This phenomenon occurs when the antibodies generated in an immune response bind to the pathogen and instead of blocking infection of cells in the body, lead to increased infection of cells and increased the amount of disease.
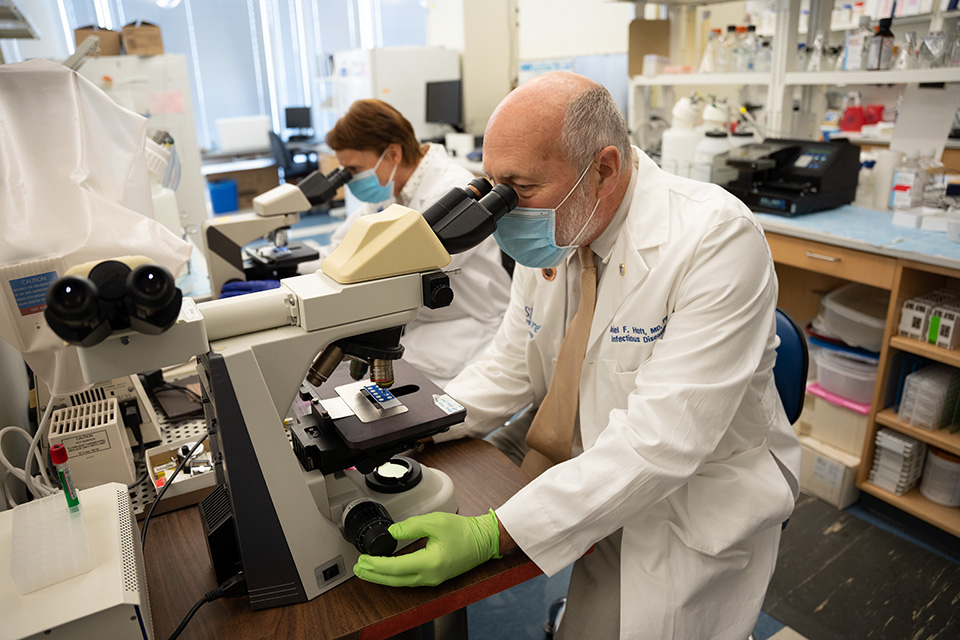
Daniel Hoft, M.D., Ph.D., director of the SLU Center for Vaccine Development, explained that antibodies have two parts — a region that recognizes what induces a response and another constant region at the end of the molecule that binds to receptors on cells. If a vaccine fails to induce antibodies directed at blocking infection of cells, but instead induces nonneutralizing antibodies that bind to the pathogen and facilitates infection of cells, the vaccine can lead to increased RSV infection among the vaccinated infants later infected with RSV.
“We think that’s probably the reason for the catastrophe,” he said. “You have to maintain the structure of the molecules in their native form so antibodies can be induced and bind to the portions that can block the virus from infecting cells.”
He explained the tragedy of the early trials, and new protein structure discoveries sparked a renewed focus that eventually cracked the code. In the years since, it has allowed for new, safer vaccine trials at SLU and other institutions throughout the world.
“There were breakthroughs that were important, both for the COVID-19 pandemic and for RSV,” he said. “RSV has been a difficult pathogen to develop a vaccine for because it normally hides its vulnerabilities, preventing the induction of optimal immunity. In addition, over the last 10 years, there’s been a greater appreciation for the importance of RSV.”
Unlocking the Shape
After a significant pause in RSV research, new studies began to emerge from scientists Barney Graham, M.D., Ph.D., and Jason McLellan, Ph.D., virologists working at the National Institutes of Health Vaccine Research Center, centered around the structure of one of the virus’s proteins — fusion glycoprotein (F). Just before this particular protein fuses with a cell, it alters its shape. Their work looked into how to lock protein F into the prefusion state, to elicit more protective antibody responses with potent neutralizing activity.
Their in-depth research of the structure of RSV F protein enhanced an interest within the scientific community around structural biology, the science of how the shape of molecules alters their function. Their research was highly relevant for understanding how to induce the most protective antibodies against the spike protein expressed by SARS-1, MERS, and SARS-CoV-2 coronaviruses. Because of the research on RSV F protein, we were ready to produce similar structural changes in the spike protein that led to much more protective antibodies against the SARS-CoV-2 pandemic viruses.
Hoft, who also led COVID-19 vaccine development at SLU, said that the discovery led to the stabilization of the spike protein that was used for the first COVID-19 vaccinations. He explained the understanding of the native molecule structure for RSV and the protein prefusion state allowed for a quicker vaccine development process during the pandemic.
“A virus does not want to make better immunogens,” Daniel Hoft said. “It wants to hide its vulnerabilities. Learning how to open up the vulnerabilities of the SARS-CoV-2 spike antigen was greatly facilitated by previous research on analogous molecules from RSV.”
The implementation of protein-structure-based design into vaccine development changed the outlook for RSV vaccines. Its early work paved the way for rapid COVID-19 vaccine development, and today’s research inches ever closer to a solution for this detrimental disease in young children.
Conducting Three Trials
The onset of the COVID-19 pandemic placed many trials on pause in the effort to quickly churn out a vaccine for the disease that infected millions throughout the world. Hoft shared that while the efforts for RSV vaccines slowed during the pandemic, the efforts were beneficial to its rapid start because the groundwork had been laid to begin RSV’s phase 3 efficacy studies.
“Once people had a chance to get vaccinated [against COVID-19], people started turning their attention back to things like RSV,” he said. “At the tail end of the emergency, we were starting to get involved in RSV vaccines because they were ready to be tested.”
The SLU Center for Vaccine Development’s Vaccine and Treatment Evaluation Units (VTEUs) served as a site for three separate phase 3 trials for RSV vaccines with principal investigators and researchers from across the University in pediatric medicine, infectious diseases, and internal medicine. The trials include an active study focused on a children’s vaccine and two studies focused on older adults.
The International Maternal Pediatric Adolescent AIDS Clinical Trials Network (IMPAACT) 2021 clinical trial specifically works with children ages 6 months to 24 months and is actively enrolling for a trial that is under the leadership of Heidi Sallee, M.D., associate professor of pediatrics in the SLU School of Medicine. The multi-site trial is in its early testing phases, as no vaccines have been officially approved for young children.
The SLU Center for Vaccine Development also hosted an international clinical trial sponsored by Bavarian Nordic. Getahun Abate, M.D., Ph.D., SLU associate professor of internal medicine, served as the trial’s principal investigator until its closure in 2023. Abate and his team worked on a recombinant protein vaccine, which acts like a natural RSV infection in order to create a long-lasting immune response.

He explained the work they conducted within the trial is key to protecting those who are at higher risk for RSV.
“There are several epidemiological studies that show that [RSV] in this age group, or the very young, leads to severe disease, hospitalizations, and even death,” Abate said. “Having a vaccine is really important to protect these high-risk groups.”
However, the trial that produced fruitful results and ultimately led to the approval of a recombinant protein vaccine for older adults was sponsored by Pfizer. Frey currently serves as SLU’s principal investigator for this study. She said initially the vaccine — called Abrysvo — was only approved for adults 60 and older.
“Globally, [RSV] is a huge problem, and there was no vaccine against it until now,” Frey said. “Another problem for children is that after RSV infection, chronic lung disease is a common complication. Lung disease can be severe, and they may have to live with impaired lung function for the rest of their lives.”
Recent developments also allowed for the vaccine’s approval among pregnant women between 32 and 36 weeks gestation during respiratory illness season (September to January). The vaccine creates critical antibodies that pass from mother to fetus, protecting the child from RSV during the first six months of life. As the first vaccine yielding protection in children, it inches RSV vaccines one step closer to safeguarding the age groups most at risk: children from birth to two years old.
A Promising Outlook Ahead
The approved vaccines for adults and pregnant women are the first major steps the industry has seen in decades. While the road to RSV vaccines has been long and arduous, the latest developments only mark the beginning of lifesavingRSV prevention and future vaccines for similarly structured respiratory viruses like COVID-19 and influenza.
To propel research forward, SLU and the Center for Vaccine Development keep the goal of finding solutions to protect high-risk groups from RSV and other respiratory illnesses at the forefront of their work. Additionally, members of the Center are forming partnerships to strengthen pediatric vaccine research in the future.
As Hoft reflected on the history and recent accomplishments of the RSV vaccine, he shared that promising opportunities lie ahead for disease prevention:
“By understanding the mechanisms important for safe and effective RSV vaccines, combined with understanding the mechanisms associated with historically poor RSV vaccine outcomes, we are in a better position to develop the best vaccines designed to protect against other important human pathogens," Hoft said.
Story by Mary Pogue, senior copywriter, Paradigm.
This piece was written for the 2023 SLU Research Institute Annual Impact Report. The Impact Report is printed each spring to celebrate the successes of our researchers from the previous year and share the story of SLU's rise as a preeminent research university. Design, photography, and some writing contributions are made by Paradigm. More information can be found here.

















